SHORT COMMUNICATION
Anti-leptospiral agglutinins in marmosets (Saguinus oedipus and Saguinus leucopus) from illegal trade
Aglutininas anti-leptospira en monos tití (Saguinus oedipus y Saguinus leucopus) de comercio ilegal
Viviana Gonzalez-Astudillo,1* M.Sc, Juliana Peña-Stadlin,2 MV, Miryam Astudillo-Hernandez,3 M.Sc.
1University of Queensland, School of Veterinary Science, Gatton QLD, 4343, Australia.
2Fundación Zoológica de Cali, Unidad de Bienestar Animal, Cra. 2 Oeste Cll. 14, Cali, Colombia.
3Universidad del Valle, Departamento de Microbiología, Av. 1N No. 3N-03, Sede Centenario, Cali, Colombia.
*Correspondence: v.gonzalez@uq.edu.au
Received: September 2014; Accepted: February 2015.
ABSTRACT
Objetive. Determine the infection status with pathogenic Leptospira of one Saguinus oedipus and nine Saguinus leucopus at the Cali Zoo that had been confiscated in Colombia from illegal trade. Materials and methods. A full physical examination, blood work, urinalysis were conducted in all individuals during the reception health check-up, in addition to running the microagglutination test with a pool of 19 serovars, with a starting dilution of 1:50. Results. A high positive titer (≥1:3200) to Leptospira alexanderi serovar manhao in an asymptomatic S. oedipus was detected. All S. leucopus tested negative or less than 1:50. Conclusions. Captive locations have been documented to artificially enhance opportunities to come into contact with contaminated bodily fluids from peridomestic rodents. However, infectious diseases acquired during the illegal transport of wildlife to major metropolitan centers are rarely considered a wildlife conservation or public health threat. Infection with zoonotic pathogens should also be considered an additional threat to endangered wild primates involved in illegal trade, which could hamper reintroduction efforts or other population management procedures for primate species with restricted and fragmented distributions.
Key words: Illegal trade, primate, serology, spirochete, zoonosis (Source: MeSH).
Objectivo. Determinar el estado de infección con Leptospira patógena en un Saguinus oedipus y nueve Saguinus leucopus en el Zoológico de Cali tras haber sido decomisados de tráfico ilegal en Colombia. Materiales y métodos. Se procedió a realizar un examen físico, cuadro hemático y bioquímica, urianálisis, y adicionalmente se realizó la prueba de microaglutinación con un pool de 19 serovares, en una dilución inicial de 1:50. Resultados. Se detectó una respuesta elevada en títulos (≥1:3200) a Leptospira alexanderi serovar manhao en un S. oedipus. Todos los S. leucopus resultaron negativos o con títulos menores de 1:50. Conclusiones. Se ha documentado que el cautiverio puede incrementar artificialmente las oportunidades para que los animales en encierros entren en contacto con fluidos corporales contaminados de roedores peridomésticos. Sin embargo, las enfermedades infecciosas adquiridas durante el transporte ilegal de la fauna silvestre a los principales centros metropolitanos son rara vez consideradas amenazas a la conservación de la fauna o para la salud pública. La infección con patógenos zoonóticos se debería también considerar como un riesgo adicional para primates en peligro de extinción involucrados en tráfico ilegal, lo que podría afectar esfuerzos de reintroducción u otras medidas de manejo de poblaciones de primates con distribuciones fragmentadas y restringidas.
Palabras clave: Espiroqueta, primate, serología, tráfico ilegal, zoonosis (Fuente: MeSH).
INTRODUCTION
Leptospirosis is a bacterial zoonosis primarily linked to the humid and warm climates of tropical regions (1). The etiological agent, Leptospira, is transmitted directly or indirectly to humans when excreted in the urine or other contaminated bodily fluids by reservoirs (mainly peridomestic rodents) (1). Epidemiologically, humans are considered dead-end hosts; however, different studies endeavor to determine the potential role of wild or zoo mammals (primarily non-human primates) as reservoirs of infection (1). Leptospira has been identified as an important and widespread pathogen detected in wildlife imported to the U.S. (1); this bacterium is of particular concern due to its capability of infecting several vertebrate genera and zoonotic risk (2). However, few studies have identified pathogens of zoonotic potential in wild animals traded illegally in Colombia. Wild animals are brought into major metropolitan areas in Colombia to be sold illegally as pets and when confiscated by environmental authorities (Environmental Police), they are brought into wildlife rehabilitation facilities, in which the final fate of the animal is to be decided (e.g. re-introduction, euthanasia, zoo collection, etc.). During their transient captivity period, wild animals can acquire infections that would be unlikely to occur in natural conditions. This has been particularly studied in non-human primates due to their generic relatedness to humans. Primates in zoological collections are spatially restricted and are brought into closer contact to maintenance hosts of zoonotic pathogens such as Leptospira spp., (1) when attracted by e.g. odors or feeding material.
Most Neotropical primates, such as callitrichids, are nearly strictly arboreal and disperse their feed; activities that have been suggested to decrease opportunities for Leptospira transmission from ground-dwelling rodents (3). However, the role of illegal trade, which has spiked over the last decades (4) and how it may enhance zoonotic pathogen transmission in wildlife in Colombia, a biodiversity hotspot, has not been thoroughly studied. Both Saguinus oedipus and Saguinus leucopus are endemic to Colombia, and are two of the most commonly trafficked primate species.
Both species are placed in conservation categories of concern (critically endangered and endangered, respectively (5)) due to the negative interplay of illegal trade, forest cover loss due to intensive colonization, and restricted geographical distribution. Infectious diseases are not currently considered as a threat to wild populations of this species, nor there have been a reported case of zoonotic pathogen transmission between trafficked animals and humans in Colombia.
MATERIALS AND METHODS
Study site. Cali Zoo is located in Cali, a major metropolitan center in the southwest of Colombia. Its coordinates are 3.4486° and 76.5586° in the northern and western latitude respectively, with an altitude of 1014 m. The local climate is defined as a tropical savanna, with an annual precipitation between 900 to 1.800 mm and an average temperature of 25°C and relative humidity of ~70% (6).
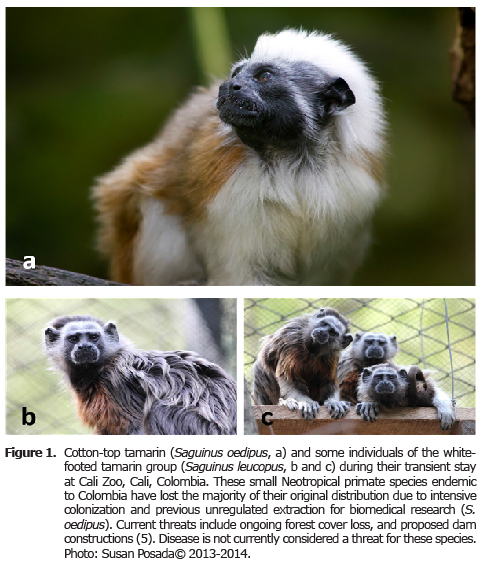
Study population, sample collection and processing. One adult female S. oedipus arrived to the Cali Zoo after being surrendered by his possessor in July 2013 to environmental authorities (Figure 1a). In February 2014 a group of nine S. leucopus arrived to the Cali Zoo after being seized by the Environmental Police (Figure 1b, 1c). All individuals from both species were chemically immobilized using ketamine (3 mg/kg IM) and midazolam (0.05 mg/kg IM) in order to receive a health check-up consisting of full physical examination, blood (CBC, biochemistry) and urine testing. Special consideration was made to detect clinical signs that have been associated with zoonotic diseases such as leptospirosis (e.g., such as weight loss, diarrhea, dehydration, anorexia, jaundice and anemia).
Handling and sample collection were performed by a veterinarian with extensive experience in Colombian captive non-domestic fauna. This study complied with the Zoological Foundation of Cali veterinary protocols, which adhere to the legal requirements of zoological collections dictated by the Colombian Association of Zoological Parks and Aquariums –ACOPAZOA, the Latin American Association of Zoological Parks and Aquariums – ALPZA, and the local department of natural resources (Autonomous Regional Corporation of Valle – CVC) in addition to the technical, scientific and administrative ethics policies in Law 84 (Colombia National Congress, 1989).
Serology testing. Approximately 200 µL of blood sera was used to conduct a microagglutination test (MAT) with 19 reference strains from the Royal Tropical Institute (Netherlands) at the Leptospirosis Diagnostic Laboratory at Universidad del Valle in Cali, Colombia. The strain pool included (L. interrogans) grippotyphosa, (L. santarosai) celledoni, (L. interrogans) pomona, (L. noguchi) australis, (L. interrogans/L. kirshneri) icterohaemorrhagiae, (L. alexanderi) manhao, (L. interrogans) bataviae, (L. borgpetersenii) sejroe, (L. noguchii) louisiana, (L. borgpetersenii) javanica, (L. santarosai) shermani, (L. interrogans) djasmin, (L. santarosai) mini, (L. interrogans) pyrogenes, (L. fainei) hurtsbridge, (L. borgpettersenii) ballum, (L. weillii) ranarum, (L. interrogans) canicola, and (L. biflexa) seramanga. Strains are subcultured weekly in Ellinghausen-McCullough-Johnson-Harris medium at 30°C. Strains are typically diluted 1:2 with buffer until a density of 6-8 x 108 spirochetes/mL is evidenced. Each of the samples were stored at -20°C and thawed via refrigeration. Aliquots of 50 µL in buffer (1X PBS, pH 7.2) were placed in the first row of a microplaque as control antigen. Each blood sera sample was placed along the remaining rows and mixed with the reference strain (antigen) arranged in columns. Microplaques were covered and incubated at 30°C for 2 hours. To evidence microagglutination, each aliquot was transferred to a glass slide and scanned by dark-field microscopy. Samples displaying a dilution ≥1:100 in which 75% of the spirochetes were agglutinated was considered positive; starting and end dilutions were 1:50 and 1:3200, respectively.
RESULTS
MAT results for all S. leucopus were negative or <1:50. In contrast, samples from the only S. oedipus yielded a titer of ≥1:3200 against L. alexanderi serovar manhao. In the same individual, further blood examination revealed an erythrocytosis and hyperproteinemia.
DISCUSSION
Evidence of hemoconcentration with hyperproteinemia is considered dehydration; an inspecific clinical sign of leptospiral infection. Ketamine HCl and midazolam have been safely used in wild S. leucopus in the past, even at higher doses (7); although how these drugs affect blood cell parameters is not well understood in this species. Thus, it is important to consider that all anesthetic agents have the potential of altering blood parameters, as well as the stress induced by the captivity and handling of a wild animal. Generally, during certain types of anesthesia, erythrocytes and leukocytes decrease due to depression of the cardiovascular system (8). Other exogenous stimuli such as stress may have an opposite effect, in which corticosteroid-induced responses from their endogenous release influence leukocyte counts more commonly than other cell lines; typically represented by lymphopenia and neutrophilia (9). In other primates, reports of anesthesia with ketamine document erythrocytosis and leukocytosis due to hemoconcentration (8), which may also explain the hyperproteinemia evidenced in our case report of anesthesia with ketamine. It is also possible that the hemoconcentration observed is due to pressor effects of ketamine, as it has been evidenced in other primates when low doses of dissociative agents are administered (8). The effects of benzodiazepine anesthesia in the blood cells of rats are primarily splenic lymphocytic depletion and low hematocrit due to increased erythrocyte destruction (10), which does not coincide with our blood and serum screening results. Despite the lack of supporting evidence of midazolam altering blood parameters in this report, it is important to consider these in future studies and perhaps compare CBC, biochemistry and serology results from paired blood and sera samples using the same anesthetic agents.
In the past, transmission experiments with Leptospira have elicited fatal disease in S. oedipus and S. geoffroyi (11), and more recently in S. labiatus (12), and in other captive callitrichids such as Callithrix kuhlii (13). Minette (3) found a serorreactive S. oedipus to serovar ballum (known to circulate in the domestic mouse, Mus spp.) among a group of eight individuals in the U.S. Reports in other marmoset species (Callithrix spp.) have found titers of up to 1:200 in asymptomatic animals (14). In 2009, Gonzalez-Astudillo et al (15) tested in Cali Zoo two Leontocebus fuscicollis that were negative or <1:50 with the MAT. However, one Cebus albifrons did test positive and underwent an asymptomatic infection eliciting low titers (1:160) to serovar australis. Another study conducted in captive primates in Colombia found titers of up to 1:1600 in an asymptomatic monkey (16). However, in the same study, six S. oedipus were negative.
It has been established already that non-human primates are more likely to acquire leptospiral infection in captivity; nevertheless, it is not known for how long titers remain detectable following a natural infection (3), and this is likely influenced by intraspecific factors or aspects inherent to the pathogen. Leptospira-infected primates can also turn into carriers (16), however this was not demonstrated in this study. Without further testing, these animals should be confined until their renal carrier state has been cleared. It is important that in future studies, when possible, asymptomatic primates with high titers are confined until their renal carrier status has been determined. Since some of the institutions receiving confiscated wildlife from the Environmental Police in Colombia are known to release animals back into their habitat, the potential to disseminate pathogens, including Leptospira spp. is a high risk for primate conservation and public health in Colombia, even if there is currently no documentation of a primate-to-human transmission or viceversa of the bacterium.
In Colombia, the infrastructure for long-term, large scale monitoring of health in wild animals is virtually inexistent and acquisition of wild animals or samples is usually opportunistic; thus, morbidity and mortality events caused by leptospirosis or any other disease can easily be overlooked. Wild animals are received in Colombia at rehabilitation centers adjunct to regional environmental entities, which determine the fate of the individual (e.g. release, euthanasia, or captivity). Due to financial and logistical constraints, testing for several pathogens is not always feasible in releasable animals. Ideally, establishing collaborations with governmental diagnostic centers in orden to conduct routinely testing with available assays. In regards to leptospirosis, incorporate MAT pools with larger numbers of serovars and serogroups in paired sampling, or other diagnostic tests (e.g. molecular techniques) to detect renal carriers as mandatory procedures in pre-release protocols as they can provide a better understanding of the infectious status of individuals. This can build baseline information that can guide future guidelines to the management of animals destined for reintroduction.
Saguinus sp. are one of the most trafficked genera in Colombia, because of their size and perceived ease of becoming tame. Despite this reality, little attention has been given to the diseases they can acquire in captivity, especially those considered threats for public health and primate conservation. This marmoset was not tested at arrival for anti-leptospiral antibodies; thus, we cannot discern when the infection occurred. However, it is possible that the marmoset got infected during its transportation to a major metropolitan center for sale, and it could have been reinfected again at Cali Zoo, eliciting this strong reaction to a serovar recognized by his immune system, and undergoing an asymptomatic infection for unknown reasons.
Occasionally, simultaneous infections with other serogroups or paradoxical reactions may interfere with determining the infecting serovar (3). In addition, there may be a species-related variability in humoral response to leptospiral infection (e.g. titer duration) (3). Although hemoconcentration of a sample may overestimate hyperimmunoglobulinemia, a titer ≥1:3200 with the MAT in combination with no visible clinical signs could suggest an undergoing infection. Another possible explanation is that continuous exposure to infection throughout life can result in an age-dependent increment in seropositivity to Leptospira (16). Past infections in non-human primates are typically associated with low titers for prolonged periods in asymptomatic individuals (17). Although the MAT precludes the establishment of the time of the infection and it is not considered a serovar-specific test because of its known cross-reactivity within serogroups (18), cases in which a single sample has elevated titers is considered diagnostic (1), and can indicate the presumptive infecting serovar (18). Although some reports exist in the literature about leptospirosis in Saguinus marmosets, to our knowledge, this is the first documentation regarding such high titers in an asymptomatic individual. It is likely that Leptospira transmission is more common that it is currently known in Colombia, as it has been demonstrated in a few seroprevalence studies in wild mammals (19) and zoological collections (15,16). In contrast, there are few citable documents about Leptospira prevalence in wildlife or zoo mammals. All marmosets were kept under observation for possible onset of symptoms and their clinical status will dictate their fate. Clinical staff and caretakers exercise biosafety measures to avoid pathogen transmission to themselves and other captive fauna.
Clinical signs associated with leptospirosis in mammals are usually non-pathognomonic (1), with reports in non-human primates documenting weight loss, diarrhea, dehydration, anorexia, jaundice, and anemia (13). The S. oedipus female in this report only elicited dehydration, perhaps due to previous exposure to the bacterium, or low virulence of the infecting serovar. The MAT detects immunoglobulin M (IgM), usually produced in the acute phase of the infection; the onset of clinical signs usually coincides with its decrease in plasma.
Cali Zoo is one of the few zoological institutions in Colombia actively investigating (14) and diagnosing leptospiral infection, amongst other disease-causing etiologies, within their collection. It is important to encourage other zoological institutions and wildlife rehabilitation centers to incorporate screening for Leptospira spp. as part of their test pool for incoming animals. This would improve the understanding of the dynamics of Leptospira in non-domestic animal species, and could lay the foundation for the improvement of the current management practices for confiscated wildlife.
Acknowledgements
This study was financially supported by the Zoological Foundation of Cali and the Leptospirosis Diagnostic Laboratory at Universidad del Valle, both in Cali, Colombia. The authors would like to thank the zoo keepers and veterinary staff at Cali Zoo, and to Mrs. Leonor Oviedo for her help with blood sera processing.
REFERENCES
1. Adler B, de la Pena-Moctezuma A. Leptospira and leptospirosis. Vet Microbiol 2010; 140(3-4):287-96.
2. Pavlin BI, Scholoegel LM, Daszak P. Risk of importing zoonotic diseases through wildlife trade, United States. Emerg Infect Dis 2009; 15(11):1721-26.
3. Minette HP. 1966. Leptospirosis in primates other than man. Am J Trop Med Hyg 1966; 15(2):190–198.
4. Ulloa A, Baptiste-Ballera LG. Editores. Rostros culturales de la fauna. 1a edición. Bogotá: Instituto de Investigación de Recursos Biológicos Alexander Von Humboldt and Instituto Colombiano de Antropologia e Historia; 2002.
5. International Union for the Conservation of Nature – IUCN. 2014 [July 20 2014]; available in: http://www.iucn.org.
6. Instituto de Hidrologia, Metereologia y Estudios Ambientales – IDEAM. 2014 [August 10 2014]; available in: http://bart.ideam.gov.co/cliciu/cali/tabla.htm
7. Savage A, Giraldo LH, Blumer ES, Soto LH, Burger W, Snowdon CT. Field techniques for monitoring cotton-top tamarings (Saguinus oedipus oedipus) in Colombia. Am J Primatol 1993; 31(3):189-196.
8. Wall HS, Worthman C, Else G. Effects of ketamine anesthesia, stress and repeated bleeding on the haematology of vervet monkeys. Lab Anim 1985; 19(2):138-144.
9. Dhabhar FS, Miller AH, McEwen BS, Spencer RL. Effects of stress on immune cell distribution – dynamics and hormonal mechanisms. J Immunol 1995; 154(10):5511-5527.
10. Elmesallamy GE, Abass MA, Ahmed-Refat NAG, Atta AH. Differential effects of alprazolam and clonazepam on the immune system and blood vessels of non-stressed and stressed adult male albino rats. Interdiscip Toxicol 2011; 4(3):132-143.
11. Noguchi H. Etiology of yellow fever. II. Transmission experiments on yellow fever. J Exp Med 1919; 29(6):565-84.
12. Reid HA, Herron AJ, Hines ME 2nd, Orchard EA, Altman NH. Leptospirosis in a white-lipped tamarin (Saguinus labiatus). Lab Anim Sci 1993; 43(3):258-9.
13. Baitchman EJ, Calle PP, James SB, Linn MJ, Raphael BL. Leptospirosis in Wied’s marmosets (Callithrix kuhlii). J Zoo Wild Med 2006; 37(2):182-5.
14. Pinna MH, Martins G, Pinheiro ACO, Almeida DS, Oria AP, Lilenbaum W. Detection of anti-Leptospira antibodies in captive nonhuman primates from Salvador, Brazil. Am J Primatol 2012; 74(1):8-11.
15. Gonzalez-Astudillo V, Wehdeking D, Pena-Stadlin JE, Arias-Bernal L, Lombo-Rodriguez DA, Astudillo-Hernandez M. Comparative seroprevalence of Leptospira interrogans in Colombian mammals along a climatic gradient. J Zoo Wild Med 2012; 43(4):768-775.
16. Romero M, Astudillo M, Sanchez J, Gonzalez L, Varela N. Titulos de anticuerpos contra Leptospira sp., en primates del zoológico Matecana, Pereira, Colombia. Rev MVZ Cordoba 2012; 17(3):3224-30.
17. Johnson MAS, Smith H, Joseph P, Gilman RH, Bautista CP, Campos KJ, et al. Enviromental exposure and leptospirosis, Peru. Emerg Infect Dis 2004; 10(6):1016-22
18. Levett PN. Usefulness of serologic analysis as a predictor of the infecting serovar in patients with severe leptospirosis. Clin Infect Dis 2003; 36(4):447–52.
19. Wells EA, D’Alessandro A, Morales GA, Angel D. Mammalian wildlife diseases as hazards to man and livestock in an area of the Llanos Orientales of Colombia. J Wild Dis 1981; 17(10):153-62.