Escherichia coli y Salmonella spp. portadoras de mcr-1 en planta de beneficio porcino, Medellín (Colombia)
Escherichia coli y Salmonella spp. portadoras de mcr-1 en planta de beneficio porcino, Medellín (Colombia)

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-CompartirIgual 4.0.
Mostrar biografía de los autores
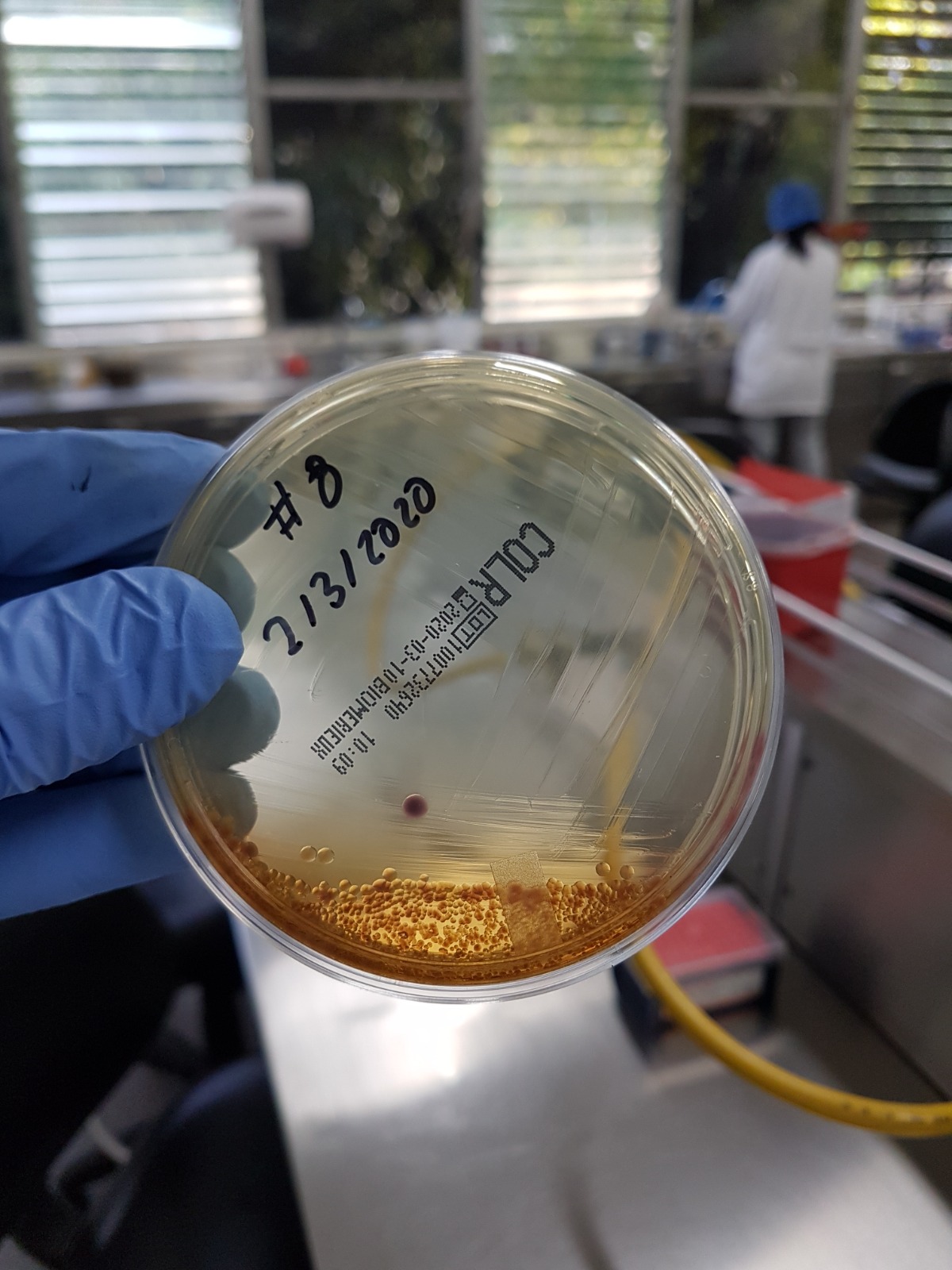
Objetivo. Evaluar la resistencia adquirida a colistina mediada por el gen mcr-1 en aislados de E. coli y Salmonella spp., de muestras de materia fecal de porcinos con destino a consumo humano en planta de beneficio animal de Medellín, Colombia. Materiales y métodos. Se realizó un estudio descriptivo, tomando 190 muestras de materia fecal de porcinos durante marzo del 2020. Para la tamización de enterobacterias resistentes a colistina se utilizó agar cromogénico y MacConkey suplementado con sulfato de colistina (2 mg/l). Los aislados fueron analizados mediante PCR para identificar el gen mcr-1, identificación bacteriana y perfil de susceptibilidad antibiótica a los aislados positivos al gen mcr-1 por el sistema automatizado Microscan®. La información fue registrada y analizada mediante estadística descriptiva. Resultados. La frecuencia de porcinos con aislados resistentes a colistina en la tamización fue del 70.52% (134/190). El 15.78% (30/190) portadores del gen mcr-1 de los cuales el 1.05% (2/190) pertenecieron a la especie Salmonella enterica y el 4.21% (8/190) E. coli. Se identificó en los aislados positivos al gen mcr-1 la capacidad de resistir la acción de múltiples antibióticos (10/10), y una E. coli con la habilidad de producir betalactamasas de espectro extendido (BLEE). La mayoría de los cerdos con enterobacterias portadoras del gen mcr-1 provenían de granjas del departamento de Antioquia, y todos en etapa de levante y ceba. Conclusiones. Este estudio evidencia la circulación del gen mcr-1 en cerdos al sacrificio, representando un riesgo potencial para la salud pública por su posible entrada a la cadena alimentaria.
Visitas del artículo 362 | Visitas PDF
Descargas
- Martinović T, Andjelković U, Gajdošik MŠ, Rešetar D, Josić D. Foodborne pathogens and their toxins. J Proteomics. 2016; 147:226-235. https://doi.org/10.1016/j.jprot.2016.04.029
- Luppi A. Swine enteric colibacillosis: diagnosis, therapy and antimicrobial resistance. Porc Health Manag. 2017; 8(3):16. https://doi.org/10.1186/s40813-017-0063-4
- Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: A microbiological and molecular biological study. Lancet Infect Dis. 2016; 16(2):161–168. https://doi.org/10.1016/S1473-3099(15)00424-7
- Olaitan AO, Morand S, Rolain JM. Emergence of colistin-resistant bacteria in humans without colistin usage: A new worry and cause for vigilance. Int J Antimicrob Agents. 2016; 47(1):1–3. https://doi.org/10.1016/j.ijantimicag.2015.11.009
- Yu CY, Ang GY, Chin PS, Ngeow YF, Yin WF, Chan KG. Emergence of mcr-1 mediated colistin resistance in Escherichia coli in Malaysia. Int J Antimicrob Agents. 2016; 47(6):504–505. https://doi.org/10.1016/j.ijantimicag.2016.04.004
- Tsuji BT, Pogue JM, Zavascki AP, Paul M, Daikos GL, Forrest A, et al. International Consensus Guidelines for the Optimal Use of the Polymyxins: Endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy. 2019; 39(1):10-39. https://doi.org/10.1002/phar.2209
- El-Sayed Ahmed M, Zhong L, Shen C, Yang Y, Doi Y, Tian G. Colistin and its role in the Era of antibiotic resistance: an extended review (2000–2019). Emerging Microbes & Infections. 2019; 9(1):868-885. https://doi.org/10.1080/22221751.2020.1754133
- Hussein NH, Al-Kadmy IMS, Taha BM, Hussein JD. Mobilized colistin resistance (mcr) genes from 1 to 10: a comprehensive review. Mol Biol Rep. 2021; 48(3):2897-2907. http://doi.org/10.1007/s11033-021-06307
- Yin W, Li H, Shen Y, Liu Z, Wang S, Shen Z, et al. Novel Plasmid-Mediated Colistin Resistance Gene mcr-3 in Escherichia coli. Mbio. 2017; 8(3):1-6. http://doi.org/10.1128/mBio.00543-17
- Carattoli A, Villa L, Feudi C, Curcio L, Orsini S, Luppi A. Novel plasmid-mediated colistin resistance mcr-4 gene in Salmonella and Escherichia coli, Italy 2013, Spain and Belgium, 2015 to 2016. Euro Surveill. 2017; 22(31):18-22. http://doi.org/10.2807/1560-7917.ES.2017.22.31.30589
- Borowiak M, Fischer J, Hammerl JA, Hendriksen RS, Szabo I, Malorny B. Identification of a novel transposon-associated phosphoethanolamine transferase gene, mcr-5, conferring colistin resistance in d-tartrate fermenting Salmonella enterica subsp. enterica serovar Paratyphi B. J Antimicrob Chemother. 2017; 72(12):3317–3324. https://doi.org/10.1093/jac/dkx327
- Wang X, Wang Y, Wang Y, Zhang S, Shen Z, Wang S. Emergence of the colistin resistance gene mcr-1 and its variant in several uncommon species of Enterobacteriaceae from commercial poultry farm surrounding environments. Vet Microbiol. 2018; 219:161-164. https://doi.org/10.1016/j.vetmic.2018.04.002
- Carroll LM, Gaballa A, Guldimann C, Sullivan G, Henderson LO, Wiedmann M. Identification of Novel Mobilized Colistin Resistance Gene mcr-9 in a Multidrug-Resistant, Colistin-Susceptible Salmonella enterica Serotype Typhimurium Isolate. mBio. 2019; 10(3):1-6. https://doi.org/10.1128/mBio.00853-19
- Qixia L, Yuan W, Yonghong X. Prevalence and transmission of mobilized colistin resistance (mcr) gene in bacteria common to animals and humans. Biosaf and Health. 2020; 2(2):71-78. https://doi.org/10.1016/j.bsheal.2020.05.001
- Valiakos G, Kapna I. Colistin Resistant mcr Genes Prevalence in Livestock Animals (Swine, Bovine, Poultry) from a Multinational Perspective. A Systematic Review. Vet Sci. 2021; 8(11):265. https://doi.org/10.3390/vetsci8110265
- Saavedra S, Díaz L, Wiesner M, Correa A, Arévalo A, Ovalle M, et al. Genomic and Molecular Characterization of Clinical Isolates of Enterobacteriaceae Harboring mcr-1 in Colombia, 2002 to 2016. Antimicrob Agents Chemother. 2017; 61(12):1-13. https://doi.org/10.1128/AAC.00841-17
- Instituto Nacional de Vigilancia de Medicamentos y Alimentos – INVIMA. Alerta por la primera detección del gen mcr-1 de resistencia al antibiótico colistín en aislamientos de Salmonella typhimurium y Salmonella give en alimentos en Colombia. Bogotá; 2017. https://app.invima.gov.co/alertas/ckfinder/userfiles/files/ALERTAS%20SANITARIAS/Alimentos_Bebidas/2017/Agosto/02-08-17%20Alerta%20colistina%20alimentos.pdf
- Ministerio de Salud y Protección Social. Circular externa conjunta No 000027 Del 14 AGO 2017. Colombia; 2017. https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/circular-externa-conjunta-n0027-de-2017.pdf
- Brito E, Hernández I, Calderón C, Hernández J, Patiño A, Pulido A, et al. Detección del gen mcr-1 en aislamientos de Salmonella spp. de animales 2006 – 2018. Revista de la Asociación Colombiana de Médicos Veterinarios Y Zootecnistas, Médicos Veterinario y Zootecnistas, ACOVEZ. 2021; 50(2):7–13. https://www.acovez.org/index.php/noticias/revistas-acovez/108-revista-acovez-no-140
- CLSI. Performance standards for antimicrobial susceptibility testing. Clinical Lab Standards Institute: USA; 2020. https://www.nih.org.pk/wp-content/uploads/2021/02/CLSI-2020.pdf
- Alkofide H, Alhammad AM, Alruwaili A, Aldemerdash A, Almangour TA, Alsuwayegh A, et al. Multidrug-Resistant and Extensively Drug-Resistant Enterobacteriaceae: Prevalence, Treatments, and Outcomes - A Retrospective Cohort Study. Infect Drug Resist. 2020; 13:4653-4662. https://www.doi.org/10.2147/IDR.S283488
- Arenas N E, Moreno V. Producción pecuaria y emergencia de antibiótico resistencia en Colombia: Revisión sistemática. Infectio 2018; 22(2):110-119. https://doi.org/10.22354/in.v22i2.717
- Nordmann P, Poirel L. Plasmid-mediated colistin resistance: An additional antibiotic resistance menace. Clin Microbiol Infect. 2016; 22(5):398–400. https://doi.org/10.1016/j.cmi.2016.03.009
- Katja H K, Roschanski N, Ruddat I, Woydt J, Hartmann M, Rösler U, Kreienbrock L. Investigation of potential risk factors for the occurrence of Escherichia coli isolates from German fattening pig farms harbouring the mcr-1 colistin-resistance gene. Int J Antimicrob Agents. 2018; 51(2):177-180. https://doi.org/10.1016/j.ijantimicag.2017.08.007
- Li XS, Liu BG, Dong P, Li FL, Yuan L, Hu GZ. The prevalence of mcr-1 and resistance characteristics of Escherichia coli isolates from diseased and healthy pigs. Diagn Microbiol Infect Dis. 2018; 91(1):63–65. https://doi.org/10.1016/j.diagmicrobio.2017.12.014
- El Garch F, de Jong A, Bertrand X, Hocquet D, Sauget M. Mcr-1-like detection in commensal Escherichia coli and Salmonella spp. from food-producing animals at slaughter in Europe. Vet Microbiol. 2018; 213:42-46. https://doi.org/10.1016/j.vetmic.2017.11.014
- Lv Z, Shen Y, Liu W, Ye H, Liu D, Liu J, et al. Prevalence and risk factors of mcr-1-positive volunteers after colistin banning as animal growth promoter in China: a community-based case–control study. Clin Microbiol Infect. 2022; 28(2):267-272. https://doi.org/10.1016/j.cmi.2021.06.033
- Institute of Medicine (US). Improving Food Safety Through a One Health Approach: Workshop Summary. Washington (DC): National Academies Press (US); 2012. https://doi.org/10.17226/13423
- Ballard A, Laramee N, Haardörfer R, Freeman M, Levy K, Caruso B. Measurement in the study of human exposure to animal feces: A systematic review and audit. Int J Hyg Environ Health 2023; 249:1-13. https://doi.org/10.1016/j.ijheh.2023.114146
- Glaize A, Young M, Harden L, Gutierrez-Rodriguez E, Thakur S. The effect of vegetation barriers at reducing the transmission of Salmonella and Escherichia coli from animal operations to fresh produce. Int J Food Microbiol. 2021; 347:109196 https://doi.org/10.1016/j.ijfoodmicro.2021.109196
- Hanning IB, Nutt JD, Ricke SC. Salmonellosis outbreaks in the United States due to fresh produce: sources and potential intervention measures. Foodborne Pathog Dis. 2009; 6:635-48. http://doi.org/10.1089/fpd.2008.0232
- Wang C, Feng Y, Liu L, Wei L, Kang M, Zong Z. Identification of novel mobile colistin resistance gene mcr-10. Emerg Microbes Infect. 2020; 9(1):508-516. http://doi.org/10.1080/22221751.2020.1732231
- Prava Rout B, Behera B, Kumar Sahu K, Praharaj I, Otta S. An overview of colistin resistance: A breach in last line defense. Med J Armed Forces India. 2023; 79(5):516-525. http://doi.org/10.1016/j.mjafi.2023.06.006
- Zhang Z, Zhao L, Song M, Luo J, Liu H, Xue K, et al. Providencia heimbachae Associated with Post-weaning Diarrhea in Piglets: Identification, Phenotype, and Pathogenesis. Curr Microbiol. 2022; 79(1):1-12. https://doi.org/10.1007/s00284-021-02697-1
- Faccone D, Moredo F, Giacoboni G, Albornoz E, Alarcón L, Nievas V, Corso A. Multidrug-resistant Escherichia coli harbouring mcr-1 and blaCTX-M genes isolated from swine in Argentina. J Glob Antimicrob Resist. 2019; 18:160-162. https://doi.org/10.1016/j.jgar.2019.03.011
- Haenni M, Poirel L, Kieffer N, Chatre P, Saras E, Metayer V, et al. Co-occurrence of extended spectrum beta lactamase and MCR-1 encoding genes on plasmids. Lancet Infect Dis. 2016; 16(3):281–182. https://doi.org/10.1016/S1473-3099(16)00007-4