Reemerging zoonoses with “One Health” approach
Las zoonosis reemergentes bajo el enfoque de “Una salud”
Show authors biography
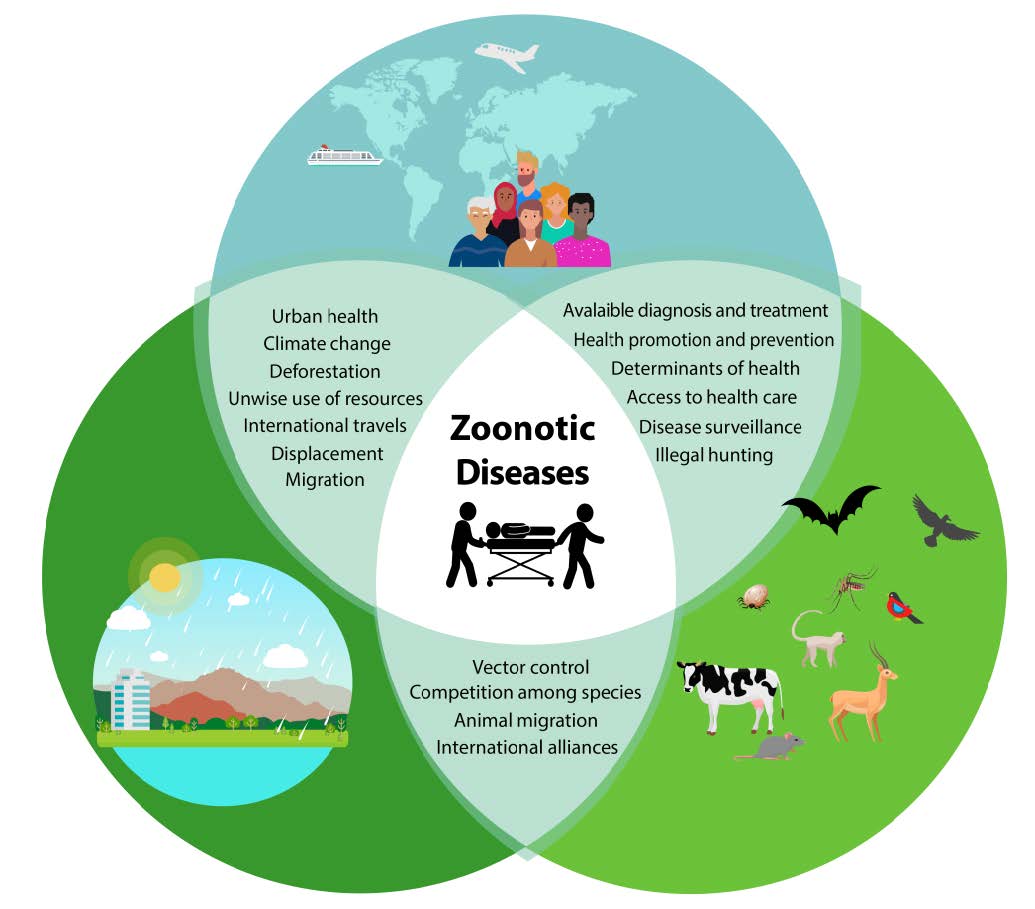
In 2004, the World Health Organization (WHO) defined emerging zoonoses as those “newly recognized or newly evolved, or that have occurred previously but show an increase in incidence or expansion in geographical, host or vector range” (1). Approximately 60% of infectious diseases affecting humans are of zoonotic origin (2), and vectors transmit almost 20% of all of them. It emphasizes the connection between human, animal, and environmental health, and the need to study these diseases in their biological, ecological, medical, and economic context to promote and guarantee health globally.
Article visits 5119 | PDF visits
Downloads
- WHO. Emerging zoonoses. [en linea]. World Health Organization: Geneva; 2004. [accessed 25.05.19]. URL Available in: https://www.who.int/zoonoses/emerging_zoonoses/en/
- Asokan G V, Asokan V. Bradford Hill’s criteria, emerging zoonoses, and One Health. J Epidemiol Glob Health. 2016; 6(3):125-129. https://doi.org/10.1016/j.jegh.2015.10.002
- OMS. El enfoque multisectorial de la OMS «Una salud». Organización Mundial de la Salud: Suiza; 2017. URL Disponible en: https://www.who.int/features/qa/one-health/es/
- Ryu S, Kim BI, Lim J-S, Tan CS, Chun BC. One Health Perspectives on Emerging Public Health Threats. J Prev Med Public Health. 2017; 50(6):411–414. https://dx.doi.org/10.3961%2Fjpmph.17.097
- Di Giallonardo F, Geoghegan JL, Docherty DE, McLean RG, Zody MC, Qu J, et al. Fluid Spatial Dynamics of West Nile Virus in the United States: Rapid Spread in a Permissive Host Environment. J Virol. 2016 Jan;90(2):862–72. https://jvi.asm.org/content/90/2/862
- OMS. Alerta y Respuesta Mundiales (GAR): De cómo los cuatro mayores brotes del siglo echan por tierra algunos mitos de gran arraigo. Organización Mundial de la Salud: Suiza; 2014. https://www.who.int/csr/disease/ebola/ebola-6-months/myths/es/
- WHO. Middle East respiratory syndrome coronavirus (MERS-CoV). World Health Organization: Geneva; 2019. https://www.who.int/emergencies/mers-cov/en/
- WHO. Emergencies preparedness, response: MERS-CoV. World Health Organization: Geneva; 2019. https://www.who.int/csr/don/archive/disease/coronavirus_infections/en/
- Chancey C, Grinev A, Volkova E, Rios M. The Global Ecology and Epidemiology of West Nile Virus. BioMed Research International. 2015; Article ID 376230. http://dx.doi.org/10.1155/2015/376230
- WHO. Emergencies preparedness, response: Severe Acute Respiratory Syndrome (SARS). World Health Organization: Geneva; 2003. https://www.who.int/csr/sars/en/
- Zhiqi Song, Yanfeng Xu, Linlin Bao, Ling Zhang, Pin Yu, Yajin Qu, et al. From SARS to MERS, Thrusting Coronaviruses into the Spotlight. Viruses. 2019; 11(1):59; https://doi.org/10.3390/v11010059
- Cheng VC, To KK, Tse H, Hung IF, Yuen KY. Two years after pandemic influenza A/2009/H1N1: what have we learned?. Clin Microbiol Rev. 2012; 25(2):223-263. https://doi.org/10.1128/CMR.05012-11
- WHO. Emergencies preparedness, response. World Health Organization: Geneva; 2019. https://www.who.int/csr/don/archive/year/2019/en/
- WHO. Emergencies. Chikungunya. World Health Organization: Geneva; 2018. https://www.who.int/emergencies/diseases/chikungunya/en/
- Vu DM, Jungkind D, Desiree LaBeaud A. Chikungunya Virus. Clin Lab Med. 2017; 37(2):371-382. https://doi.org/10.1016/j.cll.2017.01.008
- WHO. Zika virus disease. World Health Organization: Geneva; 2017. https://www.who.int/emergencies/diseases/zika/en/
- PAHO. Zika virus infection. Pan American Health Organization: Washington, D.C; 2016. https://www.paho.org/hq/index.php?option=com_topics&view=article&id=427&Itemid=41484&lang=en
- WHO. Ebola virus disease. World Health Organization: Geneva; 2019. https://www.who.int/ebola/en/
- OMS. Fiebre hemorrágica de Crimea-Congo. Organización Mundial de la Salud; Washington, D.C; 2013. https://www.who.int/es/news-room/fact-sheets/detail/crimean-congo-haemorrhagic-fever
- WHO. Emergencies preparedness, response. Yellow fever. World Health Organization: Geneva; 2019. https://www.who.int/csr/disease/yellowfev/en/
- PAHO. Yellow Fever. Pan American Health Organization: Washington, D.C; 2016. https://www.paho.org/hq/index.php?option=com_topics&view=article&id=69&Itemid=40784&lang=en
- Sarukhan A. Ébola: dos años y 11.300 muertes después: Lecciones de una epidemia para la salud global. [Accessed: 25/05/2019]. ISGlobal; 2016. https://www.isglobal.org/ebola#
- WHO. Ebola Situation Report: Democratic Republic of the Congo. [Accessed 13 June 2019]. World Health Organization: Geneva; 2019. https://www.who.int/ebola/situation-reports/drc-2018/en/
- Liu LE, Dehning M, Phipps A, Swienton RE, Harris CA, Klein KR. Clinical Update on Dengue, Chikungunya, and Zika: What We Know at the Time of Article Submission. Disaster Med Public Health Prep. 2017 Jun;11(3):290–9. https://doi.org/10.1017/dmp.2016.144
- Gould E, Pettersson J, Higgs S, Charrel R, de Lamballerie X. Emerging arboviruses: Why today? One Heal. 2017; 4:1-13. https://dx.doi.org/10.1016%2Fj.onehlt.2017.06.001
- WHO. WHO publishes list of top emerging diseases likely to cause major epidemics. [Accessed 13 June 2019]. World Health Organization: Geneva; 2015. https://www.who.int/medicines/ebola-treatment/WHO-list-of-top-emerging-diseases/en/
- Mattar VS, González TM. Mayaro and Chikungunya; two alphaviruses with clinical and epidemiological similarities. Rev MVZ Córdoba. 2015; 20:4861-4863. https://doi.org/10.21897/rmvz.1
- OPS, OMS. Alerta Epidemiológica: Fiebre de Mayaro. 1 de mayo de 2019. Organización Panamericana de la Salud / Organización Mundial de la Salud; Washington, D.C; 2019. https://www.paho.org/hq/index.php?option=com_docman&view=download&category_slug=fiebre-mayaro-2322&alias=48377-1-de-mayo-de-2019-fiebre-de-mayaro-alerta-epidemiologica-1&Itemid=270&lang=es