Veterinary perspective of the renal system in sepsis
Perspectiva veterinaria del sistema renal en la sepsis
Show authors biography
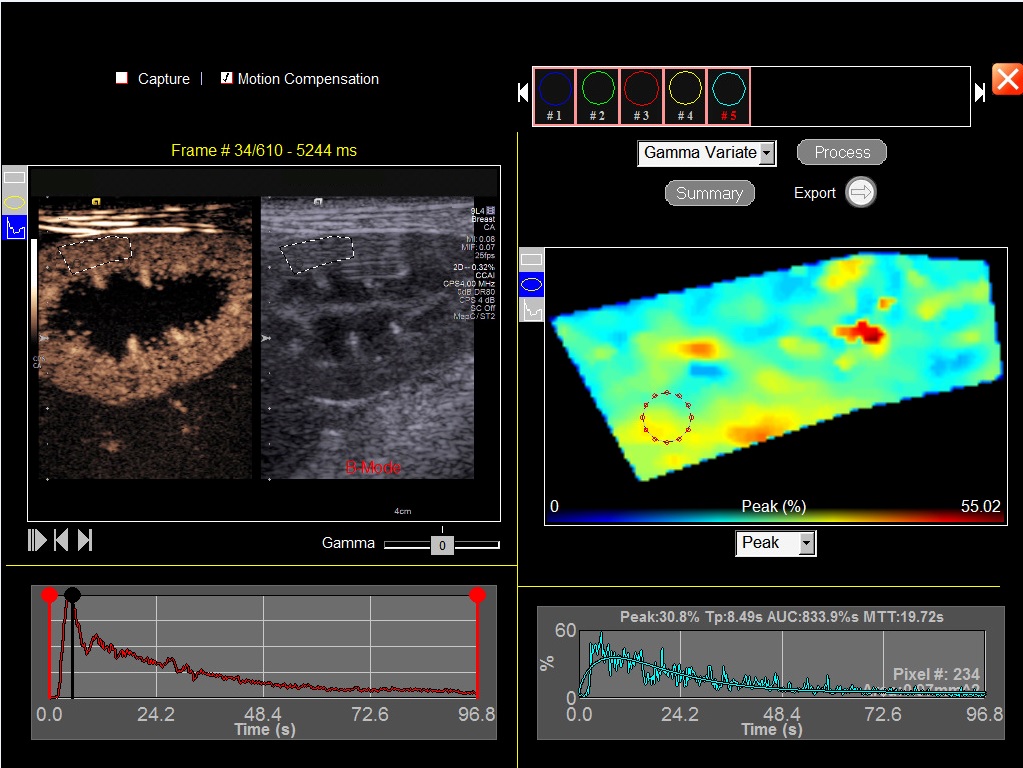
This paper aims to review, discuss and define the factors associated with development of kidney injury in patients with sepsis, diagnosis alternatives, therapy and prevention, offering to the veterinarians an updated guide to improve the prognosis of sepsis patients. Sepsis is a clinical condition that leads to systemic complications and to multiple organ dysfunction syndrome (MODS), mainly due to poor tissue perfusion in humans and animals. Acute kidney injury (AKI) is considered the most frequent and lethal among organ complications secondary to sepsis, however the etiology of AKI in patients with sepsis is complex and multifactorial and not completely elucidated. Early diagnosis of AKI is difficult and consequently the treatment is not very successful, due to hemodynamic aspects. The ultrasonography seems to be a promising exam for early diagnosis of this lesion, especially with the advent of contrast-enhanced ultrasonography (CEUS) technique, which makes possible to detect microcirculation changes in the renal parenchyma, opening the door for a variety of physiological, clinical and therapeutic applications, however, studies proving CEUS accuracy for early detection of renal damage related to sepsis in humans and animals are still necessary.
Article visits 968 | PDF visits
Downloads
- Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). J Am Med Assoc. 2016; 315(8):801–810. https://doi.org/10.1001/jama.2016.0287
- Otto CM. Sepsis in veterinary patients: What do we know and where can we go? J Vet Emerg Crit Care. 2007; 17(4):329–332. https://doi.org/10.1111/j.1476-4431.2007.00253.x
- Kenney EM, Rozanski EA, Rush JE, DeLaforcade-Buress AM, Berg JR, Silverstein DC et al. Association between outcome and organ system dysfunction in dogs with sepsis: 114 cases (2003-2007). J Am Vet Med Assoc. 2010; 236(1):83–87. https://doi.org/10.2460/javma.236.1.83
- Langenberg C, Bellomo R, May C, Wan L, Egi M, Morgera S. Renal blood flow in sepsis. Crit Care. 2005; 9(4):R363–R374. https://doi.org/10.1186/cc3540
- Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S et al. Acute renal failure in critically ill patients a multinational, multicenter study. Am Med Assoc. 2005; 294(7):813–818. https://doi.org/10.1001/jama.294.7.813
- Schneider A, Goodwin M, Bellomo R. Measurement of kidney perfusion in critically ill patients. Crit Care. 2013; 17(220):220. https://doi.org/10.1186/cc12529
- Suh SH, Kim CS, Choi JS, Bae EH, Ma SK, Kim SW. Acute Kidney Injury in Patients with Sepsis and Septic Shock: Risk Factors and Clinical Outcomes. Yonsei Med J. 2013; 54(4):965–972. https://doi.org/10.3349/ymj.2013.54.4.965
- Troìa R, Mascalzoni G, Calipa S, Magagnoli I, Dondi F, Giunti M. Multiorgan dysfunction syndrome in feline sepsis: prevalence and prognostic implication. J Feline Med Surg. 2019; 21(6):559–565. https://doi.org/10.1177/1098612X18792106
- Keir I, Kellum JA. Acute kidney injury in severe sepsis: Pathophysiology, diagnosis, and treatment recommendations. J Vet Emerg Crit Care. 2015; 25(2):200–209. https://doi.org/10.1111/vec.12297
- O’Connor PM, Evans RG. Structural antioxidant defense mechanisms in the mammalian and nonmammalian kidney: different solutions to the same problem? Am J Physiol Regul Integr Comp Physiol. 2010; 299(3):R723–R727. https://doi.org/10.1152/ajpregu.00364.2010
- Waller KR, O’Brien RT, Zagzebski JA. Quantitative contrast ultrasound analysis of renal perfusion in normal dogs. Vet Radiol Ultrasound. 2007; 48(4):373–377. https://doi.org/10.1111/j.1740-8261.2007.00259.x
- Wei K, Le E, Bin J, Coggins M, Thorpe J, Kaul S. Quantification of renal blood flow with Contrast-Enhanced Ultrasound. J Am Coll Cardiol. 2001; 37(4):1135–1140. https://doi.org/10.1016/s0735-1097(00)01210-9
- Zarjou A, Agarwal A. Sepsis and Acute Kidney Injury. J Am Soc Nephrol. 2011; 22:999–1006. https://doi.org/10.1681/ASN.2010050484
- Maddens B, Daminet S, Smets P, Meyer E. Escherichia coli pyometra induces transient glomerular and tubular dysfunction in dogs. J Vet Intern Med. 2010; 24(6):1263–1270. https://doi.org/10.1111/j.1939-1676.2010.0603.x
- LeGrand M, Bezemer R, Kandil A, Demirci C, Payen D, Ince C. The role of renal hypoperfusion in development of renal microcirculatory dysfunction in endotoxemic rats. Intensive Care Med. 2011; 37:1534–1542. https://doi.org/10.1007/s00134-011-2267-4
- Johannes T, Mik EG, Ince C. Nonresuscitated endotoxemia induces microcirculatory hypoxic areas in the renal cortex in the rat. Shock. 2009; 31(1):97–103. https://doi.org/10.1097/SHK.0b013e31817c02a5
- Zafrani L, Payen D, Azoulay E, Ince C. The Microcirculation of the Septic Kidney. Semin Nephrol. 2015; 35:75–84. https://doi.org/10.1016/j.semnephrol.2015.01.008.
- Singel DJ, Stamler JS. Chemical physiology of blood flow regulation by red blood cells: The role of nitric oxide and S-Ntrosohemoglobin. Annu Rev Physiol. 2005; 67:99–145. https://doi.org/10.1146/annurev.physiol.67.060603.090918
- Adembri C, Sgambati E, Vitali L, Selmi V, Margheri M, Tani A et al. Sepsis induces albuminuria and alterations in the glomerular filtration barrier: a morphofunctional study in the rat. Crit Care. 2011; 15:R277. https://doi.org/10.1186/cc10559
- Doi K, Yuen PST, Eisner C, Hu X, Leelahavanichkul A, Star RA. Reduced production of creatinine limits its use as marker of kidney injury in sepsis. J Am Soc Nephrol. 2009; 20:1217–1221. https://doi.org/10.1681/ASN.2008060617
- Zappitelli M. Epidemiology and diagnosis of acute kidney injury. Semin Nephrol 2008; 28(5):436–446. https://doi.org/10.1016/j.semnephrol.2008.05.003
- Lisowska-myjak B. Serum and Urinary Biomarkers of Acute Kidney Injury. Blood Purif. 2010; 29:357–365. https://doi.org/10.1159/000309421
- Ostermann M, Joannidis M. Acute kidney injury 2016: diagnosis and diagnostic workup. Crit Care. 2016; 20:1–13. https://doi.org/10.1186/s13054-016-1478-z
- Kovarikova S. Urinary biomarkers of renal function in dogs and cats: a review. Praha:Vet Med. 2015; 60(11):589–602. https://doi.org/10.17221/8527-VETMED
- Koyner JL. Assessment and Diagnosis of Renal Dysfunction in the ICU. Chest. 2012; 141(6):1584–1594. https://doi.org/10.1378/chest.11-1513
- Lee YJ, Hu YY, Lin YS, Chang CT, Lin FY, Wong ML et al. Urine neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute canine kidney injury. BMC Vet Res. 2012; 8(248):1–9. https://doi.org/10.1186/1746-6148-8-248
- Winkler MS, Nierhaus A, Rösler G, Lezius S, Harlandt O, Schwedhelm E et al. Symmetrical (SDMA) and asymmetrical dimethylarginine (ADMA) in sepsis: High plasma levels as combined risk markers for sepsis survival. Crit Care. 2018; 22(1):1–10. https://doi.org/10.1186/s13054-018-2090-1
- Dahlem DP, Neiger R, Schweighauser A, Francey T, Yerramilli M, Obare E et al. Plasma Symmetric Dimethylarginine Concentration in Dogs with Acute Kidney Injury and Chronic Kidney Disease. J Vet Intern Med. 2017; 31(3):799–804. https://doi.org/10.1111/jvim.14694
- Köster LS, Peda A, Fraites T, Sithole F. A preliminary investigation into the prognostic relevance of symmetric dimethylarginine in critically ill dogs. J Vet Emerg Crit Care. 2018; 28(6):527–531. https://doi.org/10.1111/vec.12780
- Godin M, Murray P, Mehta RL. Clinical approach to the patient with AKI and sepsis. Semin Nephrol. 2015; 35:12–22. https://doi.org/10.1016/j.semnephrol.2015.01.003
- Langenberg C, Bagshaw SM, May CN, Bellomo R. The histopathology of septic acute kidney injury: a systematic review. Crit Care. 2008; 12(2):1–7. https://doi.org/10.1186/cc6823
- Wan L, Bagshaw SM, Langenberg C, Saotome T, May C, Bellomo R. Pathophysiology of septic acute kidney injury: What do we really know? Crit Care Med. 2008; 36(4):S198–S203. https://doi.org/10.1097/CCM.0b013e318168ccd5
- Morrell ED, Kellum JA, Pastor-soler NM, Hallows KR. Septic acute kidney injury: molecular mechanisms and the importance of stratification and targeting therapy. Crit Care. 2014; 18:501. https://doi.org/10.1186/s13054-014-0501-5
- Hinshaw LB, Taylor FB Jr, Chang AC, Pryor RW, Lee PA, Straughn F et al. Staphylococcus aureus-induced shock: a pathophysiologic study. Circ Shock. 1988; 26(3):257-265. https://europepmc.org/article/med/3061682#abstract
- Takasu O, Gaut JP, Watanabe E, To K, Fagley RE, Sato B et al. Mechanisms of cardiac and renal dysfunction in patients dying of sepsis. Am J Respir Crit Care Med. 2013; 187(23):509–513. https://doi.org/10.1164/rccm.201211-1983OC
- Chvojka J, Sykora R, Krouzecky A, Radej J, Varnerova V, Karvunidis T et al. Renal haemodynamic, microcirculatory, metabolic and histopathological responses to peritonitis-induced septic shock in pigs. Crit Care. 2008; 12:R164. https://doi.org/10.1186/cc7164
- Ravikant T, Lucas CE. Renal blood flow distribution in septic hyperdynamic. J Surg Res. 1977; 22:294–298. https://doi.org/10.1016/0022-4804(77)90146-9
- Lima A, Rooij TV, Ergin B, Sorelli M, Ince Y, Specht PAC et al. Dynamic Contrast-Enhanced Ultrasound identifies microcirculatory alterations in sepsis-induced acute kidney injury. Crit Care Med. 2018; 20(8):1–9. https://doi.org/10.1097/CCM.0000000000003209
- Santos RV, Merlini NB, Souza LP, Machado VMV, Pantoja JCF, Prestes NC. Doppler ultrasonography in the renal evaluation of bitches diagnosed with pyometra before and after treatment with ovariohysterectomy. Pesqui Vet Bras. 2013; 33(5):635–642. https://doi.org/10.1590/S0100-736X2013000500014
- Lerolle N, Guérot E, Faisy C, Bornstain C, Diehl JL, Fagon JY. Renal failure in septic shock: predictive value of Doppler-based renal arterial resistive index. Intensive Care Med. 2006; 32:1553–1559. https://doi.org/10.1007/s00134-006-0360-x
- Granata A, Zanoli L, Clementi S, Fatuzzo P, Di Nocolò P, Fiorini F. Resistive intrarenal index: myth or reality? Br J Radiol. 2014; 87:1–7. https://doi.org/10.1259/bjr.20140004
- Donia MA, Gomaa NA, Abdelmegeid M, Nassif MN. Biomarkers versus duplex ultrasonography for early detection of acute kidney injury in dogs: an experimental study. Slov Vet Res. 2019; 56:179–186. https://doi.org/10.26873/SVR-755-2019
- Gullichsen E, Nelimarkka O, Halkola L, Ninikoski J. Renal oxygenation in endotoxin shock in dogs. Crit Care Med. 1989; 17:547-50. https://doi.org/10.1097/00003246-198906000-00013
- Kalantarinia K, Okusa M. Ultrasound Contrast Agents in the Study of Kidney Function in Health and Disease. Drug Discov Today Dis Mech. 2007; 4(3):153-158. https://doi.org/10.1016/j.ddmec.2007.10.006
- Seiler GS, Brown JC, Reetz JA, Taeymans O, Bucknoff M, Rossi F et al. Safety of contrast-enhanced ultrasonography in dogs and cats: 488 cases (2002-2011). J Am Vet Med Assoc. 2013; 242(9), 1255–1259. https://doi.org/10.2460/javma.242.9.1255
- Fischer K, Meral FC, Zhang Y, Vangel MG, Jolesz FA, Ichimura T et al. High-resolution renal perfusion mapping using contrast-enhanced ultrasonography in ischemia-reperfusion injury monitors changes in renal microperfusion. Kidney Int. 2016; 89:1388–1398. https://doi.org/10.1016/j.kint.2016.02.004
- Girlich C, Jung EM, Iesalnieks I, Schreyer AG, Zorger N, Strauch U et al. Quantitative assessment of bowel wall vascularisation in Crohn’s disease with contrast-enhanced ultrasound and perfusion analysis. Clin Hemorheol and Microcirculation. 2009; 43:141–148. https://doi.org/10.3233/CH-2009-1228
- Zeisbrich M, Kihm LP, Druschler F, Zeier M, Schwenger V. When is contrast-enhanced sonography preferable over conventional ultrasound combined with Doppler imaging in renal transplantation? Clin Kidney J. 2015; 8:1-9. https://doi.org/10.1093/ckj/sfv070
- Haers H, Saunders JH. Reference Point ultrasonography in dogs. J Am Vet Med Assoc. 2009; 234:460–470. https://doi.org/10.2460/javma.234.4.460
- Miyoshi T, Okayama H, Hiasa G, Kawata Y. Contrast-enhanced ultrasound for the evaluation of acute renal infarction. J Med Ultrason. 2015; 43(1):141–143. https://doi.org/10.1007/s10396-015-0655-z
- Schneider AG, Hofmann L, Wuerzner G, Glatz N, Maillard M, Meuwly JY et al. Renal perfusion evaluation with contrast-enhanced ultrasonography. Nephrol Dial Transplant. 2012; 27(2):674–681. https://doi.org/10.1093/ndt/gfr345
- Dong Y, Wang W, Cao J, Fan P, Lin X. Quantitative Evaluation of Contrast-Enhanced Ultrasonography in the Diagnosis of Chronic Ischemic Renal Disease in a Dog Model. PLoS One. 2013; 8:1–7. https://doi.org/10.1371/journal.pone.0070337
- Brenner M, Schaer GL, Mallory DL, Suffredini AF, Parillo JE. Detection of renal blood flow abnormalities in septic and critically ill patients using a newly designed indwelling thermodilution renal vein catheter. Chest. 1990; 98:170–179. https://doi.org/10.1378/chest.98.1.170
- Mannucci T, Lippi I, Rota A, Citi S. Contrast enhancement ultrasound of renal perfusion in dogs with acute kidney injury. J Small Anim Pract. 2019; 60(8):1–6. https://doi.org/10.1111/jsap.13001
- Gasser B, Uscategui RAR, Maronezi MC, Pavan L, Simões APR, Martinato F et al. Clinical and ultrasound variables for early diagnosis of septic acute kidney injury in bitches with pyometra. Sci Rep. 2020; 10(1):1–12. https://doi.org/10.1038/s41598-020-65902-4
- Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017; 43(3):304–377. https://doi.org/10.1007/s00134-017-4683-6
- Poston JT, Koyner JL. Sepsis associated acute kidney injury. BMJ. 2019; 364:k4891. https://doi.org/10.1136/bmj.k4891
- Honore PM, Jacobs R, Hendrickx I, Bagshaw SM, Boyau OJ, Boer W et al. Prevention and treatment of sepsis ‑ induced acute kidney injury: an update. Ann Intensive Care. 2015; 5:51. https://doi.org/10.1186/s13613-015-0095-3
- Giantomasso D Di, Morimatsu H, May CN, Bellomo R. Intrarenal blood flow distribution in hyperdynamic septic shock: Effect of norepinephrine. Crit Care Med. 2003; 31:2509–2513. https://doi.org/10.1097/01.CCM.0000084842.66153.5A
- McClellan JM, Goldstein RE, Erb HN, Dykes NL, Cowgill LD. Effects of administration of fluids and diuretics on glomerular filtration rate, renal blood flow, and urine output in healthy awake cats. Am J Vet Res. 2006; 67(4):715–22. https://doi.org/10.2460/ajvr.67.4.715